Orthopedic Devices
|
|
|
Internal Fixation - plates |
|
|
|
|
|
|
|

|
Fracture Fixation continued...
by Tim B Hunter, MD, MSc
Internal Fixation continued...
Plates
Most fracture fixation plates are made of stainless steel or titanium and can be used for both flexible and rigid fracture
fixation (figure: fracture fixation plates). Flexible
fixation means the fracture fragments displace in
relation to each other when a load is applied
across the fracture site. There is appreciable interfragmentary
movement under a functional load. The majority of
the fracture fixation methods commonly employed use flexible or "biologic" fixation. Fracture healing under
flexible fixation typically occurs by means of
callus formation.
Compression fixation techniques, which are less common, produce rigid fixation. Rigid fracture fixation with plates and screws is desirable for fractures that involve an articular
surface. Articular fractures require
exact anatomic reduction and stable fixation
to avoid development of abundant callus. This is
important because unevenness of the joint surface
and presence of callus formation at the articular
surface lead to patient discomfort and often development
of early and progressive osteoarthritis
(Ruedi, 2007).
Bridging of any fracture with a stiff
splint reduces mobility of the fracture fragments,
which allows minimal displacement under a functional
load. Although rigidity of the fracture fixation contributes to reducing fracture mobility, the
only technique that can effectively abolish motion
at a fracture site is interfragmentary compression of the fracture fragments.
However, with proper placement and use of plates and screws there is often enough stability to diminish the strain at the fracture site to such
extent there is direct healing without formation
of visible callus.
Terminology commonly used with
fracture plating is “compression plating” and “neutralization plating” (figure: neutralization and buttress plates; figure: buttress plate with bone substitute). Compression plating
applies compression to the fracture ends. Severely comminuted fractures and/or fractures with bone loss prevent compression plating. In these cases, the
fixation plate is applied in neutral mode to hold the fracture
fragments in place without compression during healing. No matter the case,
frequently not all the screw holes in a fracture fixation plate are
filled.
Back to Top
Back to Top
Plates continued...
Buttress plates are used more for bony alignment rather than compression. They are indicated for situations in which the fracture fragments are unstable in compression or axial loading. They are most commonly found in the distal radius and in the proximal tibia where they stabilize tibial plateau fractures (figure: buttress plate with bone substitute; figure tibia buttress plate). They are also sometimes found in distal femur intercondylar fractures (figure: femur buttress plate).
Plates
are most commonly used for fixation of long
bones, but they also are used in the spine and for
arthrodesis of the wrist (figure: wrist arthrodesis) (Ruedi, 2007; Benjamin, 1994). When diaphyseal fractures in the long
bones are treated with a fixation plate, a minimum of six
cortices should be engaged at each fracture site,
except for the femur, which requires eight.
Dynamic compression plates (DCPs) were
introduced in 1969 and have since been modified for multiple applications.
These plates produce axial compression at the fracture site,
which is achieved by means of oval holes designed to provide compression of the fracture as eccentrically placed screws are tightened on either side of the fracture line. DCPs are designed to compress fracture fragments together rather than merely hold them in contact. They are typically used for fractures that are stable (figure: fibula dynamic compression plate).
Dynamic compression plates function
in different modes: compression, neutralization, tension band, and buttress. They are available in
different sizes to accommodate fracture
fixation in bones of different sizes. The screw
holes in DCPs are oval and are best described
as a portion of an inclined and angled cylinder.
DCP plates can be used with different types of
screws. The areas about the plate
holes are less stiff than the areas between them,
and during bending the plate tends to bend only
at the hole sites (Ruedi, 2007; Benjamin, 1994).
A newer design of DCPs is the low-contact
DCP (LCD), which reduces the area of contact “footprint” between the plate and bone. This design
produces less compromise to the capillary
network of the periosteum, which leads to a relative
improvement in cortical perfusion (figure: wrist arthrodesis with LCD).
The distribution of the holes and even stiffness of
this plate allow gentle and elastic deformation of
the entire plate without stress concentration at
one of the screw holes, as occurs with the standard DCP.
The footprint of the low-contact DCP has a trapezoidal
shape, and the screws can be inserted in
the plate in different modes: compression, neutral,
and buttress (Ruedi, 2007; Benjamin, 1994; Berquist, 1995; Freiberg, 2001; Hunter, 2001).
One-third tubular plates are thinner than DCPs. Tubular plates are called “tubular” because
they form part of the circumference of a
tube, that is, one-third, one-fourth, and so forth
of the circumference of a tube or cylinder. Tubular
plates have a radiographic appearance similar
to that of DCPs. These plates are only 1 mm
thick and are used for fracture fixation in regions
with a small amount of overlying soft tissue, such
as the distal fibula, distal ulna, and olecranon.
The holes in tubular plates are oval and are surrounded
by small collars, which allow a certain
degree of eccentric screw placement and which
prevent screw head penetration of the plate (Benjamin, 1994; Hunter, 2001).
Blade plates are fixed angle plates. They have a
sharply angled extension at the end that is placed
into the metaphysis. Blade plates have a wide
range of angles to accommodate different fixation
needs (figure: blade plates) (Ruedi, 2007; Benjamin, 1994; Wiss, 2013; Berquist, 1995; Freiberg, 2001; Hunter, 2001).
Reconstruction plates have deep notches between
the holes and allow a considerable amount
of bending (figure: uniplanar external fixator; figure: fixation plates; figure pelvis reconstruction plates). These plates are often generically referred to as malleable fixation plates. The screw holes are
oval to allow for dynamic compression.
Reconstruction
plates are used mainly for fixation of
pelvic and acetabular fractures. They can also be
used for fixation of distal humeral, clavicular, and finger
fractures (figure: clavicle reconstruction plate; figure: finger reconstruction plate) (Ruedi, 2007; Benjamin, 1994; Wiss, 2013; Berquist, 1995; Freiberg, 2001; Hunter, 2001).
Interfragmentary bone compression with a
plate can be achieved by compression with a tension
device, by compression with a DCP or low-
contact DCP, by contouring (over-bending) the
plate, and by using additional screws through
plate holes. An interfragmentary screw should be
used whenever fracture fragments permit it.
Placement of the interfragmentary screw through
the plate is preferred over a freestanding placement (figure: femur blade plate and interfragmentary screw)
(Ruedi, 2007).
In situations where there is a highly comminuted fracture or deficient bone stock a periarticular locking plate and screws may be used. There are locking screw holes combined with the compression plate allowing the plate to be used as both a locking device and a fracture compression device (figure: humerus periarticular locking plate with bone substitute; figure: humerus periarticular locking plate; right femur periarticular plate; figure: tibia periarticular plate and bone substitute. Periarticular locking plates may also have varying thickness, greater in the diaphysis and thinner in the metaphysis.
Bridge plates are used for fixation of complex diaphyseal fractures to minimize additional soft
tissue injury. A bridge plate is applied through
minimal soft-tissue exposure. It is designed to
span a critical fracture area and is fixed with
screws to the bone fragments only near its two
ends (Ruedi, 2007).
The point contact fixator (PC-Fix) was
initially designed for fixation of forearm bone
fractures. It consists of a narrow plate with a specially
designed undersurface with small points
that come in contact with the bone surface. The
plate is fixed to bone with unicortical self-tapping
screws. If needed, the PC-Fix plate can be gently
contoured to accommodate the shape of the
bone.
The LISS (less invasive stabilization system) plate was
designed for fracture fixation in the metaphyseal
and diaphyseal regions, initially for the distal femur
and later for the proximal tibia (figure: femur LISS plate). Its
shape conforms to the anatomic contour of a specific
area of bone. Therefore separate implants
are available for the left and right sides. Additional
contouring is not needed because the LISS plate does not need to touch the bone. The plate
is fixed to the bone with locked unicortical screws
placed by means of a minimally invasive submuscular
approach. Before placement of a PC-Fix or
LISS plate, the fracture must be adequately reduced.
PC-Fix and LISS plates have several
promising advantages over conventional plates,
including better preservation of the blood supply to
bone and better resistance to infection. They provide
a fixed-angle plate screw device that consists
of two components for easy application in complex
fractures and self-tapping cortical screws that
are easily and rapidly applied to a reduced fracture.
The additional advantage of a LISS plate is
its insertion in a minimally invasive fashion (Collinge, 2000; Kregor, 2001; Frigg, 2001; Kregor, 2002).
A variety of special anatomically shaped plates
exists that are dedicated for fracture fixation in a
specific location. Some of these are the condylar
plate 95° for stabilization of proximal and distal
femoral fractures, angled blade plate 120° for valgus
osteotomy of the femur, condylar buttress
plate for the distal femur, T-plate 4.5 for the
proximal humerus and proximal tibia, lateral
tibial head buttress plate, tibial head buttress
plate (right and left), cobra head plate for arthrodesis
of the hip, angled blade plate for the femur, dynamic condylar screw for the
proximal and distal femur (combination of side
plate and a separate screw), and an oblique angled 3.5 T-plate for fixation of distal radius fractures (figure: wrist T-plate; figure: variable angle volar distal radius locking plate).
A somewhat prominent special anatomically shaped periarticular plate is the olecranon plate used as part of an elbow plating system, most commonly for comminuted fractures of the proximal ulna nvolving the olecranon and coronoid. It is also used for osteotomies of the olecranon (figure: olecranon plate and screws and radial head prosthesis). The olecranon plate is intended to provide stable fracture fixation and preserve the blood supply. These plates are precontoured for anatomic fit. The proximal spoon shapted portion of the plate is slightly thinner than the shaft portion.
The clavicle hook plate is a clavicular plate with a hook engaging below the acromion (figure: clavicle hook plate). It is intended for fixation of both lateral clavicle fractures and acromioclavicular joint injuries (Synthes). The plates are precontoured as left and right plates and are available with 6 or 8 holes, one of which is an anterolateral screw hole for additional options for screw fixation in the lateral clavicle. The dynamic compression screw holes accept 3.5 mm cortex or 4.0 mm cancellous bone screws. The offset hook design is intentional to avoid insertion of the hook into the acromioclavicular ligament. The plate achieves a high percentage of bony unions and a low percentage of complications, but there are concerns about possible long-term complications involving the acromioclavicular joint (Tiren, 2012; Gaetke-Udager, 2019). A similar hook design is sometimes used in other locations, such as with distal ulnar fractures (figure: distal ulnar hook locking compression plate).
Medial open wedge high tibial osteotomy is a well-established procedure for the treatment of medial knee joint osteoarthritis and symptomatic varus malalignment. Puddu or TomoFix plates systems are specifically designed for use with osteotomies close to the knee, particularly the high tibial osteotomies for treatment of medial compartment knee arthritis or sometimes for opening wedge distal femoral varus osteotomies for treatment of lateral compartment knee arthritis (Puddu, 2007) (figure: tibial osteotomy plate; figure: Puddu titanium plate with hydroxyapatite bone graft wedge).
Total or partial wrist fusion is sometimes performed for severe carpal osteoarthritis. In this regard, a spider plate may be used for partial carpal arthrodesis (figure: spider plate). Modular plate systems are available for four-corner and other limited wrist fusions for osteoarthritis, complex fractures, revision of failed previous wrist fusions, marked carpal instability, or rheumatoid arthritis (figure: Acumed hub cap fusion plates).
The next step in the evolution of biologic plating
is percutaneous plating, which results in less
surgical trauma to tissues and further improvement
in clinical results compared with current
methods of open surgical plate insertion. The percutaneous technique was
developed in an effort to combine the advantages
of intramedullary nailing with the more stable
fracture fixation available with plating. In percutaneous
plating, a smaller incision is used to place
the plate, and the screws are then placed percutaneously.
Preliminary reports about the results of
percutaneous plating are promising. However,
these methods are technically challenging, and long-term results from prospective studies will be
needed for definite assessment of their advantages
and disadvantages (Ruedi, 2007; Collinge, 2000).
When fracture fixation plates are evaluated radiographically, important
considerations are where the plate is located,
whether the plate symmetrically spans the fracture,
and the degree of fracture reduction. The
plate should not impinge on joint motion, and the
plate and the screws should not violate the articular
surface of a joint. Any malposition or migration of the
plate, breakage of the plate or screws, or loosening of the plate
should be reported. The major possible
complication with conventional plating is potential
compromise of cortical blood supply because
of a large contact area between the plate and underlying
cortex (Ruedi, 2007).
Back to Top
| Fixation plates |
Fixation plates |
Intramedullary rods and nails |
Neutralization and buttress plates |
 |
 |
 |
 |
| From Benjamin, 1994 |
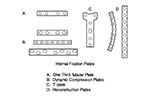
A - one third tubular plate; B - dynamic compression plate (DCP); C- T-plate; D - reconstruction plates. From Benjamin, 1994 |
Locking femoral intramedullary rods: A - reconstruction rods; B - intramedullary hip screw; C - supracondylar rod. From Benjamin, 1994 |
From Benjamin, 1994 |
 |
| Wrist arthrodesis with low contact dynamic compression plate |
Clavicle hook plate |
Spider plate for partial wrist arthrodesis |
 |
 |
 |
 |
| From Taljanovic, 2005 |
|
The scaphoid has been removed. The spider plate transfixes the lunate, triquetrum, capitate, and hamate which are partially fused. From Taljanovic, 2005 |
 |
| Olecranon plate and screws plus unipolar radial head prosthesis |
 |
 |
 |
 |
| 35 year-old man who fell and sustained comminuted olecranon and radial head fractures. He was treated with olecranon plate and screws as well as a unipolar radial head prosthesis. Courtesy Lana Hirai Gimber, MD, MPH |
 |
| Acumed Hub Cap Fusion Plates |
Ulnar hook locking compression plate |
|
 |
 |
 |
|
| These plates are designed for four-corner and other wrist fusions. Image from Acumed |
53 year-old woman with distal right radial and ulnar fractures. There is an ulnarly applied hook locking compression plate and screws and a variable angle volar distal radius locking plate and screws. |
|
Back to Top
|