|
Orthopedic Devices
|
| |
|
|
|
Joint Arthroplasty - Wrist and Hand |
|
|
|
| |
|
|
|
|

|
Joint Arthroplasty - Wrist & Hand
by Tim B Hunter, MD, MSc
Wrist Arthroplasty
Wrist arthrodesis, either partial or total, is the standard surgical treatment for a painful arthritic
wrist (figure: wrist arthrodesis with low contact dynamic compression plate; figure partial wrist arthrodesis with spider plate). However, total wrist arthroplasty (TWA) may be applicable in some cases, because improvements in
biomaterial technology and surgical technique have made wrist arthroplasty a good alternative for patients who might have had an arthrodesis. Wrist arthroplasty offers increased wrist function, and the more modern prostheses and surgical techniques promise less associated complications and a longer functional lifespan for the prosthesis.
�Total wrist arthroplasty is designed to reduce pain and improve function in patients with disabling wrist destruction from rheumatoid arthritis, post-traumatic arthritis, and advanced degenerative osteoarthritis (Nair, 2014). The contraindications for total wrist arthroplasty and for arthroplasty in the finger joints are
not clearly defined. Acute and chronic wrist and hand infections preclude arthroplasty surgery. It is usually precluded in patients with lack of sensory or motor function and in patients with particularly poor bone stock. Chronic severe volar and ulnar subluxation at the wrist as well as the need for weight bearing through the wrist joint (use of a cane or walker) are also considered contraindications. Flail nonfunctional digits with swan-neck deformity, failed arthroplasties of the metacarpophalangeal
(MCP) or interphalangeal joints,
and lupus arthropathy are also relative contraindications for wrist arthroplasty or for further surgery in the hand (Berquist, 1995; Taljanovic, 2003).
Intact extensor carpi radialis brevis
and longus tendons is requisite for total
wrist arthroplasty. The carpal height and alignment must be maintained or reconstructed as part of the arthroplasty. The third metacarpal bone is most important. It is
often used as a center of rotation in the coronal
plane. Stemmed distal prosthetic components
are usually inserted into the third metacarpal.
The carpal alignment should be restored
to the neutral position in relationship with
the radius, but palmar and dorsal flexion is acceptable on the lateral view (Taljanovic, 2003).
Wrist extension with ulnar deviation for a power grip is probably the most important
motion of the wrist to be preserved or restored as much as possible (Taljanovic, 2003).
Wrist arthroplasties typically allow 60° of extension,
40° of flexion, and 20° of radial and ulnar
deviation (Berquist, 1995; Carlson, 1998; Berger, 1999). The distal ulna is
always resected to avoid ulnar abutment that
occurs after resecting the distal radius. The proximal
radial component of the prosthesis is usually not cemented into the radius, while the distal component, which usually goes into the third metacarpal, is often cemented.
There are several designs for wrist and finger arthroplasties with evolution of the designs over the last several decades (Nair, 2014). This evolution has been stimulated by two factors. First, arthroplasty in the wrist and hand provide good relief from pain and improved function for patients with severe, destructive arthritis. Second, wrist and hand arthroplasties while initially successful, have poor long term results with osteolysis, subsidence, and implant fractures after 10 years. This is particularly true of the first generation implants from the 1960's and 1970's which used a Silastic spacer only (figure: Silastic finger joint implants; figure: second metacarpophalangeal joint silicone implant; figure: various Silastic implants) (Calenoff, 1973;Swanson, 1968).
Second generation wrist implants used metal ball and socket or hemispherical designs but still had considerable soft tissue and mechanical problems. Third generation wrist implants have tri-spherical and other articular surfaces (figure: third generation wrist arthroplasty). Fourth generation wrist implants are mainly uncemented and use porous surfaces for better osteointegration (Nair, 2014). It can be difficult to distinguish the various generation of wrist and hand arthroplasties, and their exact names are hard to remember and are unimportant per se. It is important to understand their function and potential complications.
The terms elastomer, silicone, and Silastic are
commonly used in describing joint implants, especially implants in the hand, wrist, and foot for treatment of severe rheumatoid arthritis. Elastomer is a type of synthetic
rubber, and silicone and Silastic are types of
polymers. As a practical matter these materials cannot be distinguished from each other with certainty on
radiographs. Silastic is used more than
elastomer and silicone in current orthopedic
practice and can be found in repair of almost any
deformity in any joint. While it is probably not technically correct to do so, it is not that uncommon for authors to use silicone and Silastic interchangeably. Another term often encountered is UHMWPE (ultra-high molecular weight polyethylene). It is often used for articular surface interfaces in many joint implants.
The modern era for wrist and finger arthroplasty began in the 1960's with the first generation implants. Specifically, in 1968, Swanson announced a double-stemmed, flexible-hinge silicone wrist prosthesis (Swanson, 1968). This first generation prosthesis was basically a spacer
around which scar tissue formed with soft
tissue stability to the joint. This prosthetic joint gave good relief of symptoms and range of motion, but as noted above, it had a high complication rate. It and similar early silicone joints are no longer used.
In the
1970s, Muely and Volz simultaneously invented
metal and plastic wrist devices for cement fixation of the components. These second generation designs had metal components
for insertion into the second and third metacarpals
as well as into the distal radius. Loosening of the distal component occurred
in over 50% of these prostheses (figure: 2nd generation wrist implant). In 1973, Volz introduced an articulated nonhinged prosthesis
which functioned as a dorsopalmar tracking device. No rotational motion was allowed. While this design had fewer complications, tendon balance and dislocations continued to be significant problems (Berquist, 1995; Carlson, 1998; Berger, 1999).
To overcome the significant problems with ball and socket
type wrist arthroplasty, a new third generation semiconstrained,
transversely oriented, ellipsoid wrist prosthesis
was introduced
by Beckenbaugh in 1982, and it is known
as the biaxial total wrist arthroplasty (figure: third generation wrist arthroplasty). The prosthetic stems are coated with porous
material to enhance cement fixation or eliminate the need for it. This prosthesis has a mean cumulative survival for revision after seven years of 81% with patients having good pain relief and improved motion. However, there is a high complication rate as with earlier total wrist arthroplasty designs and a worrying amount of loosening after 5 years (van Harlingen, 2011).
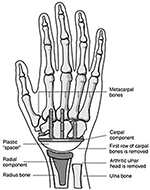
Numerous additional "fourth generation" designs for total wrist arthroplasty
have been proposed in an attempt
to solve the complications with previous models. Most fourth generation implants are uncemented, though many offer the option to use cement for fixation (Weiss, 2013). A typical fourth generation design has three components-radial stem, carpal plate, and carpal ball (figure: ReMotion total wrist arthroplasty; figure: wrist arthroplasty components; figure: fourth generation wrist implant). Another common design uses a silicone
elastomer implant at the wrist together with a titanium metal grommet (figure: silicone wrist implant with titanium grommet; figure: silicone and metal grommet wrist and finger implants).
It is difficult to keep track of these different designs. What is important is to realize radiocarpal arthroplasty is used in patients with end-stage destructive arthritis, usually rheumatoid arthritis, to good initial effect, but there are long term complications with osteolysis, loosening, and disruption of the prosthesis. All elbow, wrist, and finger arthroplasties suffer from these possibilities, and imaging evaluation of them should always look for early signs of prosthesis failure.
Occasionally, a limited arthroplasty is performed
in the carpus with replacement of one or more of the carpal bones, most often the scaphoid or lunate (figure: trapezium prosthesis). Sometimes a limited carpal bone fusion is performed using a SLIC (scapholunate intercarpal) screw fixation system (figure: SLIC screw system).
In general, these procedures have poor outcomes because of
the difficulty in maintaining the intricate balance
of the wrist, which relies on both the bones and
the functional complex system of intrinsic and
extrinsic wrist ligaments. Silastic and metal arthroplasties
of the thumb carpometacarpal joint after
the trapezium resection have sometimes been performed. As with other arthroplasties involving the wrist, they have had variable results.
A standard treatment for thumb (1st) carpometacarpal osteoarthritis is trapeziectomy. The thumb length and pinch strength are preserved by filling the trapezium space with hematoma, tendon, silicone graft, fabric patches, or bone graft (Petscavage-Thomas, 2019). Ligament reconstruction tendon interposition (LRTI) arthroplasty is a combination of volar ligament reconstruction, trapeziectomy, and tendon interposition. On radiography there is trapeziectomy and a tunnel in the base of the thumb (1st) metacarpal for passage of an interposed tendon. A tunnel in the base of the thumb metacarpal may also indicate volar ligament reconstruction. Tunnels in the first and second metacarpals and partial or total trapeziectomy may be a result of suspenionplasty for treatment of thumb base arthritis. Instead of tendons being pulled through a bony tunnel, there can be tightrope fiber wire fixed by Endobuttons to the first metacarpal base and second metacarpal as part of the suspension (Petscavage-Thomas, 2019).
The distal ulna on rare occasions is resected due to significant trauma or for treatment of a malignant tumor. To restore as much function as possible for the forearm and wrist there may be reconstruction of the distal radioulnar (DRU) joint with a variety materials - methylmethacrylate, Silastic polymer, or metal (figure: methylmethacrylate DRU; figure: Silastic ulnar head prosthesis; figure: DRU metal hemiarthroplasty). In these situations a hemiarthroplasty is performed with resection of the ulnar head (or even the distal ulnar shaft) and articulation of the prosthetic ulnar head with the native carpal bones. A more complete distal radioulnar joint prosthesis is the APTIS DRUJ prosthesis, which is an enclosed joint semiconstrained prosthesis for the distal radioulnar joint in which there is end-stage wrist arthritis from trauma or inflammatory change (figure: APTIS prosthesis). The long term outcome of these procedures remains to be seen, but they are often the only possibility for the patient to have preservation and meaningful use of the upper extremity.
Back to Top
Hand Arthroplasty
Metacarpophalangeal (MCP) and proximal interphalangeal
joint (PIP) arthroplasties are performed for severe joint destruction, most commonly from rheumatoid arthritis. Both
silicone and metal prosthetic designs are used (figure: Silastic metacarpophalangeal joint arthroplasties). These may be stand alone procedures or used in combination with surgery in other joints, most often joint arthrodesis in the interphalangeal joints (figure: Herbert screw joint arthroplasty).
An arthroplasty
is occasionally performed for an isolated
MCP or proximal interphalangeal joint (PIP) affected by osteoarthritis (figure: silicone second MCP arthroplasty; figure: combined silicone metal second MCP arthroplasty). In cases of rheumatoid arthritis, arthroplasty of the PIP
joints is rarely indicated. If surgery is contemplated, arthrodesis is usually performed. In addition, arthrodesis is much more commonly
performed than arthroplasty for arthritic pain relief in the
distal interphalangeal joints.
There are numerous
designs for MCP and PIP joint arthroplasty. Sometimes resection
arthroplasty with a silicone elastomer spacer
placement is performed in the MCP or
PIP joints (figure: silicone second MCP arthroplasty). Surgical fusion of the metacarpophalangeal joints is rarely performed. The modern Swanson design for MCP
implants and PIP implants remains standard (figure: Swanson joint implants). This is a silicone
prosthesis that is often used with circumferential titanium
grommets if there is adequate bone
stock. Variations of this design are found in other types of MCP joint arthroplasties with or without metal grommets (figure: NuFlex MCP joint system).
Arthroplasty for the MCP and PIP joints can provide good pain relief and sometimes restore mobility (Bales, 2014). Unfortunately, the long term outcome has been relatively unchanged for several decades. The pain relief and range of motion achieved after surgery is good, but it does not mirror the success of large joint arthroplasty (Adkinson, 2014). The long term hope of many investigators and surgeons is for innovations in biotechnology to make joint prostheses obsolete, but this point is not close at hand, and we will see ever more designs for joint arthroplasties, particularly in the upper extremity where they have not received the widespread usage and success evident with hip and knee replacement.
Forearm, wrist, hand, and finger reconstructions are occasionally performed using artificial tendons. The artificial tendons are sometimes opaque enough to be visible on radiographs or may be impregnated with barium for visibility (figure: Hunter tendon rod). They are also visible on CT and MRI imaging and may produce strange imaging effects or artifacts that are difficult to initially recognize if one does not have a history of such tendon placement.
Back to Top
| Distal ulna and distal radioulnar joint reconstruction with Rush rod and methylmethacrylate |
Silastic ulnar head prosthesis in a patient with end stage rheumatoid arthritis |
Second generation total wrist arthroplasty and Silastic metacarpophalangeal (MCP) implants. |
 |
 |
 |
 |
| 66 year-old woman with distal ulnar resection for treatment of a leiomyosarcoma
|
|
The wrist is malaligned in ulnar deviation. There is extensive remodeling in the long (3rd) finger metacarpal. Metal grommets with Silastic implants are at the thumb and long finger MCP joints. From Benjamin, 1994. |
 |
| Distal radioulnar joint hemiarthroplasty |
Third generation "biaxial" total wrist prosthesis |
 |
 |
 |
 |
| 66 year-old man who fell from ladder with multiple injuries to the left elbow, left forearm, and left wrist. A distal radioulnar hemiarthroplasty restores the ulnar aspect of the left wrist joint. There are fracture fixation plates in the radial and ulnar shafts. A variable pitch headless screw stabilizes a scaphoid fracture. |
52 year-old woman with rheumatoid arthritis and left total wrist prosthesis which failed three years later and was replaced by a wrist arthrodesis. The distal stem of the prosthesis protruded out of the left 3rd metacarpal. The radiograph of the left wrist arthrodesis shows 2nd-5th MCP Swanson silicone arthroplasties, most of which are at least partially displaced. On the patient's right side there are also extensive changes of rheumatoid arthritis with multiple failed Swanson silicone MCP prostheses (see below images). |
 |
| APTIS DRUJ (distal radioulnar joint) prosthesis |
Fourth generation Total wrist arthroplasty (ReMotion Total wrist) |
Typical wrist arthroplasty components |
 |
 |
 |
 |
| 70 year-old woman with past fractures of distal radius and ulna and development of positive ulnar variance and disabling ulnar abutment syndrome. |
|
Image reproduced with permission from OrthoInfo. © American Academy of Orthopaedic Surgeons http://orthoinfo.aaos.org/
|
 |
| Fourth generation total wrist arthroplasty (TWA) |
|
 |
 |
 |
|
| 69 year-old woman with rheumatoid arthritis. fourth generation wrist arthroplasty. There are also Silastic implants of the 2-5th proximal interphalangeal joints which are failing. |
|
 |
| Wrist arthrodesis with low contact dynamic compression plate |
Spider plate |
Second metacarpophalangeal joint silicone arthroplasty |
 |
 |
 |
 |
| From Taljanovic, 2005 |
The scaphoid has been removed. The spider plate transfixes the lunate, triquetrum, capitate, and hamate which are partially fused. From Taljanovic, 2005 |
|
 |
| Silicone trapezium prosthesis |
Flexible wrist carpal bone fusion screw (SLIC screw repair system) |
Herbert screws used for proximal interphalangeal joint arthrodesis |
Silastic joint implants |
 |
 |
 |
 |
| From Taljanovic, 2005 |
|
From Taljanovic, 2005 |
55 year-old woman with severe rheumatoid arthritis. Silastic implants replace the 2nd through 5th metacarpophalangeal joints. There is an arthrodesis at the thumb metacarpophalangeal joint with three K-wires, a tension band, and a splint. |
 |
| NeuFlex MCP Joint Implant System |
Antibiotic laden cement spacer |
Right hand and wrist silicone and titanium metal grommet prostheses |
Swanson silicone and metal joint prostheses |
 |
 |
 |
 |
| Middle-aged woman with rheumatoid arthritis. The implants contain a flexible, tear-resistant silicone rubber. |
36 year-old man with loss of index finger and a portion of the third metacarpal from a gunshot wound. The antibiotic laden cement block is stabilized by a small malleable plate and screws for treatment of third metacarpal bone infection. |
67 year-old woman with advanced, destructive rheumatoid arthritis in the hands and wrists. |
There are radiocarpal and 2nd-5th metacarpophalangeal joint arthroplasties using silicone with titanium grommets. From Taljanovic, 2005 |
 |
| Multiple failed metacarpophalangeal Swanson silicone arthroplasties |
Left second metacarpophalangeal joint combined metal silicone arthroplasty |
Flexor digitorum Hunter rod tendon reconstruction |
 |
 |
 |
 |
| 52 year-old woman with severe rheumatoid arthritis in the right hand and wrist. There are multiple failed MCP Swanson silicone prostheses with partial displacement and bone fracturing. There is surgical arthrodesis at the right index finger MCP joint and bony fusion from long standing arthritis in the wrist and thumb MCP joint. In her left hand and wrist there was failure of a wrist prosthesis and failure of MCP joint arthroplasties (see above images). |
75 year-old man with severe osteoarthritis at the left index finger metacarpophalangeal joint. |
64 year-old man with planned staged flexor digitorum tendon reconstruction using a Hunter rod (arrow). |
Back to Top
|